Emergency Medical and Integrated Healthcare Services

Emergency Medical and Integrated Healthcare Services (EMIHS) is part of the MCFRS Division of Operations. Working closely with the Maryland Institute for Emergency Medical Services Systems (MIEMSS), our local fire and rescue corporations, career and volunteer labor representatives, the Fire and Emergency Services Commission (FESC), the Montgomery County Department Health and Human Services (HHS), the County Medical Society, and other stakeholder agencies within county government, EMIHS is responsible for:
- overseeing the delivery of Basic Life Support (BLS) and Advanced Life Support (ALS) treatment and transportation services
- administering in-county Mobile Integrated Healthcare (MIH) initiatives
- developing MCFRS policies applicable to EMS
- providing Quality Improvement (QI) and Quality Assurance (QA) oversight for in-county EMS care
- participating in the development and administration of EMS training initiatives
- defining EMS equipment specifications
- ensuring effective EMS communications systems coordination
- providing operations support (e.g. secondary response, quality assurance, etc.) for all emergency response providers
- ensuring MCFRS compliance with the Health Insurance Portability and Accountability Act (HIPAA) and federal and state regulations
- administering the majority of MCFRS’ legal obligations relating to the retention and disclosure of patient care and other operational reports and records
Over the course of forty plus years, pre-hospital medicine (commonly called Emergency Medical Services or EMS) in the United States has evolved. In the late 60’s, the first standardized Emergency Medical Technician (EMT) curriculum came into existence which was notable specifying a minimum set of specific skills and qualifications. Later, in the early 70’s, an Emergency Medical Technician – Paramedic curriculum also came into existence. The MCFRS was instrumental in the development of both of these standards of care in the state of Maryland.
Since that time, EMS has progressed. Scope of practice has greatly expanded, minimum skills, training, and education have increased, and traditional fire departments have gradually accepted the reality that aside from law enforcement, EMS has (and remains) the primary reason why our residents call for emergent help. In many respects, we have evolved into an “EMS-based fire department.” The MCFRS prides itself on providing outstanding and rapid treatment and transport for patients suffering from time dependent medical emergencies such as heart attacks, strokes, traumatic injuries and cardiac arrests. We remain firmly committed to this aspect of our EMIHS program.
However, the MCFRS has come to understand that sometimes patients with frequent calls to 911 have unfulfilled chronic needs and has instituted a Mobile Integrated Health (MIH) program to better meet serve these patients. MIH addresses the growing disparity between the volume of emergency 911 calls we respond and the limited availability of our EMS resources. Through partnerships with local hospitals, the health department, and various community groups, MIH works to pair these patients with a variety of existing community-based medical and social programs. The net result is these users are better served because they ultimately receive more appropriate types and levels of healthcare which meet their specific needs. And, emergency response capabilities remain available to serve our residents who are experiencing high priority emergency medical events.
Since MIH works in tandem with EMS, it makes sense that our name reflects our current mission: Emergency Medical and Integrated Healthcare Services.
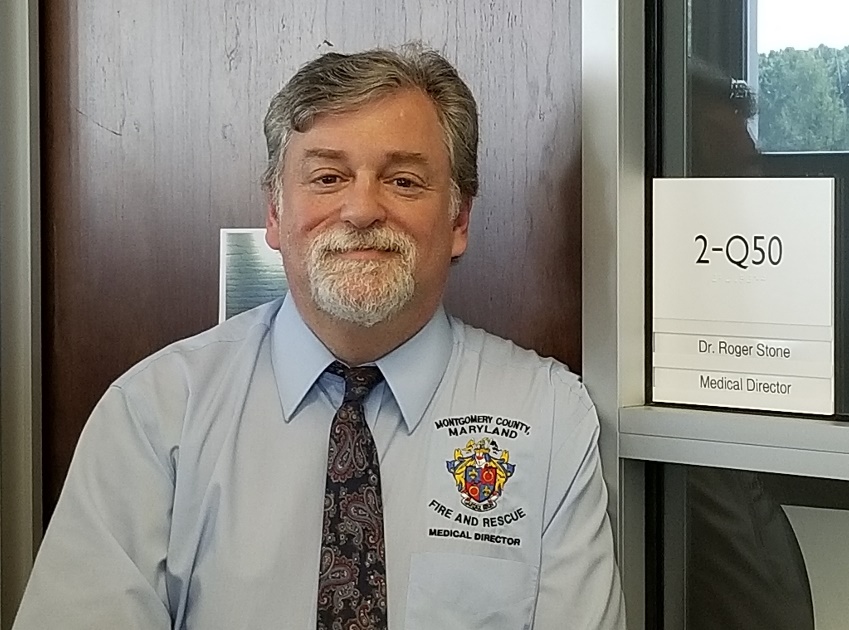
EMIHS Section Staff
- Captain Zachary Grossman, Assistant Quality Assurance Officer
- Captain Jeffrey Kane, Assistant Quality Assurance Officer
- Captain Wes Shipley, Assistant Quality Assurance Officer
- Lieutenant Athena Hollenbach, Assistant Quality Assurance Officer
- Lieutenant Will Tipton, Assistant Quality Assurance Officer
- Captain Nicholas Wagner, Quality Improvement Officer
- Lieutenant Luke Rush, Assistant Quality Improvement Officer
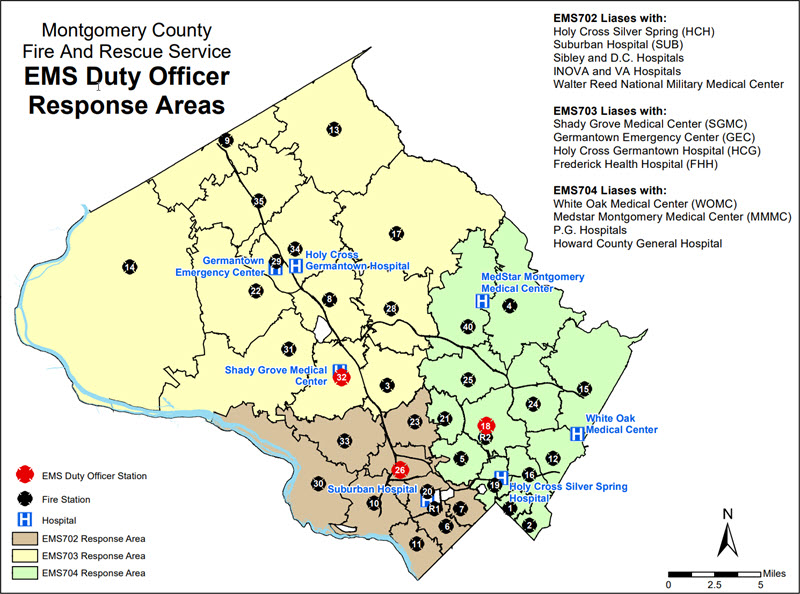
Emergency Medical Services (EMS) Duty Officers and Response Areas
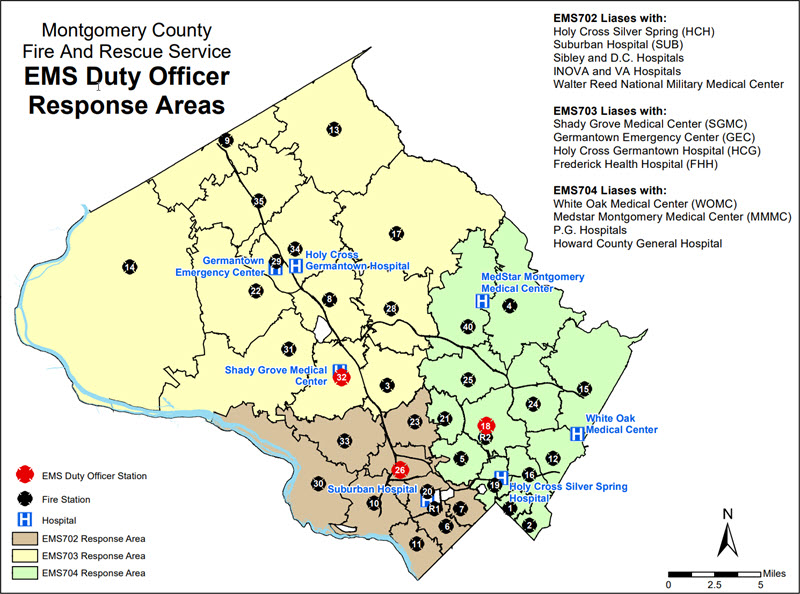
-
EMS 701 (Station 19)
- Lieutenant Luke Rush (A-Shift)
- Lieutenant Mark Grant (B-Shift)
- Lieutenant Will Tipton (C-Shift)
-
EMS 703 (Station 32)
- Captain Yann Le Renard (A-Shift)
- Captain Dwayne Dutrow (B-Shift)
- Captain Jeff Kane (C-Shift)
-
EMS 704 (Station 25)
- Captain Wesley Shipley (A-Shift)
- Captain Patrick Dillon (B-Shift)
- Captain Zachary Grossman (C-Shift)
-
EMS 705 (Station 34)
- Lieutenant Justin Hoover (A-Shift)
- Lieutenant Athena Hollenbach (B-Shift)
- Lieutenant Brennan Martin (C-Shift)
-
EMS Duty Officer - Relief
- Captain Jason Giza
- Lieutenant Brett Carter

Mobile Integrated Health Program
MCFRS’ Mobile Integrated Health program identifies frequent callers to 911 and strives to avert unnecessary ambulance transports, emergency department visits, and hospital admissions/readmissions, while ultimately improving patient outcomes. Experience has shown that when a citizen accesses 911 several times within a short time frame, there are often larger unmet needs that must be addressed. The focus of this program is to identify specific healthcare resources our frequent callers of 911 need and, through direct engagement, leverage those resources through an interagency partnership with the Montgomery County Department of Health and Human Services, our six local hospitals, and a variety of public and private care providers. Clients enter our program through a referral-based system. Referrals typically come from our EMS providers and hospital partners.
Program Manager: Avital Graves, MBA, MHA, NRP
[email protected]
Staff:
- Ms. Pilley Doe, RN, MIH Community Health Nurse